ABOUT PRIMARY HYPEROXALURIA TYPE 1 (PH1):
What is primary hyperoxaluria type 1 (PH1)?
A PH1 diagnosis can be overwhelming. It's OK to have questions. The good news is, even though it's a rare condition, you're not alone. Learn about how PH1 affects the body, genetic testing, and more.
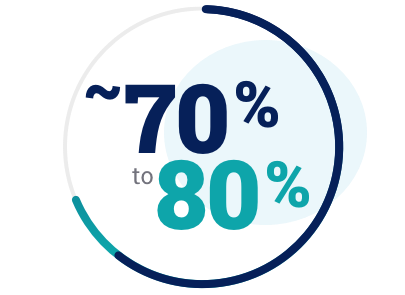
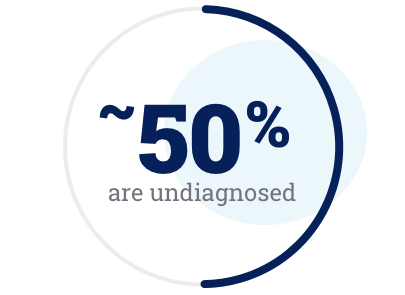
How prevalent is PH1?
Primary hyperoxaluria is a rare, inherited, autosomal recessive, and progressive disease that causes the overproduction of oxalate. Normally, oxalate is present only in small amounts, is not used by the body for anything, and is primarily eliminated by the kidneys.
PH1 Perspectives: Describing PH1

Sign up
Join the community taking on PH1. You’ll receive relevant information on your condition, plus a water bottle.
Sign up & join us
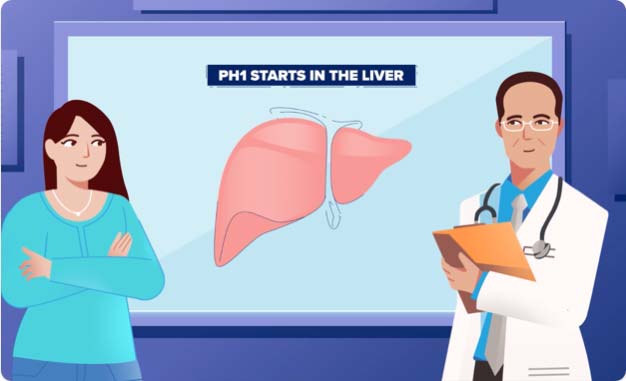
What causes PH1?
Normally, glycolate oxidase (GO) and alanine:glyoxylate aminotransferase (AGT) enzymes in the liver work together to regulate levels of oxalate. In PH1, AGT is broken, and GO continues to work and make the building blocks for oxalate. This leads to the overproduction of oxalate.
Watch how this happens, below:

Oxalate is a waste product that cannot be further broken down or used by the body, and is primarily eliminated by the kidneys.

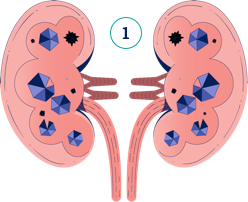
How does PH1 affect the kidneys?
In PH1, oxalate is constantly being overproduced by the liver, and the kidneys cannot keep up with removing it. Watch the video below to understand how damage can occur:

Oxalate is constantly overproduced and can cause continuous damage that gets worse over time. Diagnosing PH1 as early as possible can help you take steps to manage it.

What are the common signs of PH1?
Although kidney stones are the most common, and often the first sign of PH1, not all people with PH1 will have stones. When you have PH1, your kidneys are at risk for damage even if you are not getting stones.
In fact, PH1 may present in a number of ways:
Having any kidney stones,
even only one, as a child
Having repeated kidney stone episodes (recurrent kidney stones)
Nephrocalcinosis (finding crystals in kidney tissue during a renal evaluation)
End-stage kidney disease (kidney failure)
Failure to thrive
(not growing sufficiently as a baby)
These are not all the possible signs, symptoms, or complications of PH1, and not all people with PH1 exhibit them at the same times. Having one of these signs or symptoms does not necessarily mean that you or a loved one have PH1. Your doctor is your most important source of information if you ever have questions about your health.
PH1 Perspectives: How I got my PH1 diagnosis

There was just blood in his urine.
He had no other symptoms, but you could see that he was in pain. I remember he had a lot of stones in his kidney when he first got diagnosed.
Build a personalized PH1 discussion guide
If you or a relative of yours has a history of kidney stones, or other signs that make you curious about PH1, you can answer 6 quick questions to receive a personalized discussion guide. Once completed, you can bring it to your healthcare provider to discuss if you or your loved one should be tested for PH1.
Or you can download, print, and answer the PH1 discussion guide questions.
What are some of the symptoms I could experience?
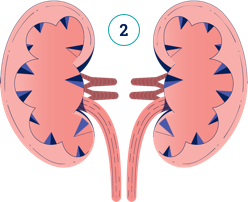
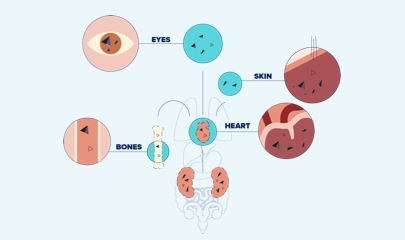
Patients with PH1 may experience different symptoms at different times in life; some will experience symptoms as babies, while others may not have symptoms until later in life. While symptoms vary from person to person, oxalate is always overproduced in the body and can cause damage to the kidneys and other organs.
Kidney stone symptoms can include:
- Pain in the side of the body
- Dysuria (painful urination)
- Hematuria (blood in the urine)
- Urinary tract infections (UTIs)
If you think you are experiencing these symptoms, consider contacting your doctor or a urologist.
These are not all the possible symptoms of a kidney stone.
Symptoms of end-stage kidney disease (ESKD) can include:
- Producing little or no urine
- Feeling ill and tired
- Loss of appetite, nausea, and vomiting
- Pale skin color
- Swelling of the hands and feet
- In PH1, decreased kidney function that can lead to oxalate depositing throughout the body
These are not all the possible symptoms of end-stage kidney disease.
If you think you are experiencing these symptoms, consider contacting your doctor or a nephrologist. By keeping track of your kidney health, you and your doctor can make more informed decisions.
Can someone in my family have PH1, too?
PH1 is an autosomal recessive disease that is passed down within families. That's why it is important that family members, especially siblings, of a person with PH1 should consider getting tested for the disease.

PH1 can affect members of the same family in different ways, including how the disease presents itself and/or how it progresses.
If a healthcare provider suspects PH1, they may recommend a test to measure the amount of oxalate in the urine or blood, as a first step toward diagnosis.
Or a healthcare provider may recommend that family members be tested with a genetic test (a method doctors use to help confirm a PH1 diagnosis through a blood or saliva sample) to aid in determining if they have the disease. If you are an immediate family member of a person with PH1, speak with your doctor about whether genetic testing makes sense for you.
Your doctor is your best source of information if you ever have questions about your health.
SEE ONE OPTION FOR GENETIC TESTING
If you haven’t been diagnosed with PH1, you or your healthcare provider can request genetic testing and counseling through the Alnylam Act® program offered at no charge, if you meet certain criteria. The test is done using a blood, saliva, or buccal sample. Siblings and family members may also be tested through Alnylam Act®. The Alnylam Act® program was created to provide access to genetic testing and counseling to patients as a way to help people make more informed decisions about their health.
While the program is sponsored by Alnylam Pharmaceuticals, all services are performed by independent third parties. For more information and program rules, download a brochure at AlnylamActPH1.com.
PH1 Perspectives: Experience with Genetic Testing


Download a PH1 Handbook
You can customize and download your own PH1 Handbook, which provides an overview of PH1 management, monitoring, and more.

So, what’s next?
Explore ways you and your care team can help you take on PH1.
learn about Management